Take into consideration waking as a lot as info of a mysterious illness spreading in a distant nook of the world. The indicators are imprecise—fever, fatigue, maybe a rash—nonetheless the speed at which it’s transferring by communities is alarming. Inside weeks, it’s not solely a headline; it’s on the doorstep, tough each factor we thought we knew about worldwide properly being security. This isn’t science fiction—it’s the reality of rising infectious illnesses (EIDs) in 2025. From norovirus surges inside the U.S. to Oropouche virus outbreaks in journey hubs, the world is grappling with new and re-emerging pathogens that demand swift, coordinated movement. On this weblog submit, we’ll dive into the dynamic panorama of EIDs, uncover how the worldwide neighborhood is responding, and supply insights on what we’re capable of do to stay ahead of the curve. Buckle up—it’s a wild expertise by science, protection, and human resilience.
What Are Rising Infectious Sicknesses?
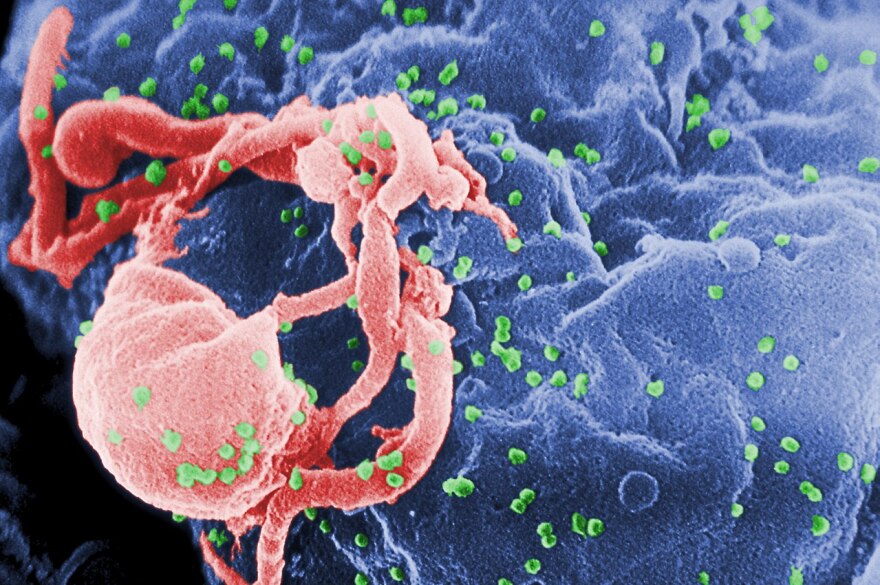
Rising infectious illnesses are infections which have simply currently appeared in a inhabitants, are rapidly rising in incidence, or are spreading to new geographic areas. Take into account them as uninvited guests on the worldwide properly being get collectively—some are utterly new, like SARS-CoV-2, whereas others, like drug-resistant tuberculosis, are outdated foes carrying new disguises. According to the World Properly being Group (WHO), EIDs can stem from beforehand unknown pathogens, acknowledged brokers spreading to new areas, or re-emerging illnesses that resurface after a decline. The stakes are extreme: given that Nineteen Seventies, over 40 new infectious illnesses have been acknowledged, along with Ebola, Zika, and COVID-19. These illnesses don’t respect borders, and their capability to unfold rapidly in our hyper-connected world makes them a worldwide concern.
I keep in mind volunteering at a neighborhood properly being clinic all through the early days of the COVID-19 pandemic. The uncertainty was palpable—victims had been scared, healthcare workers had been stretched skinny, and no one knew what was coming subsequent. Which have taught me how shortly a model new pathogen can upend lives and why understanding EIDs is important. In 2025, we’re seeing illnesses like norovirus GII.17 outpacing its cousin GII.4 inside the U.S., with outbreaks rising from beneath 10% in 2022–23 to 75% in 2024–25, in response to the Services for Sickness Administration and Prevention (CDC). Within the meantime, illnesses like Oropouche virus, with a median incubation interval of merely 3.2 days, are popping up in travel-associated cases, reminding us that worldwide mobility fuels these outbreaks.
Why Are EIDs on the Rise in 2025?
The surge of EIDs isn’t occurring in a vacuum—it’s pushed by a perfect storm of human, environmental, and natural parts. Picture a bustling metropolis the place people, animals, and microbes are in mounted contact, and likewise you’ve acquired a recipe for sickness emergence. Proper right here’s a breakdown of why EIDs are gaining flooring:
- Worldwide Journey and Commerce: With air journey doubling since 2000, a pathogen can hop continents in hours. The Johns Hopkins Medication journey properly being info notes that vacationers to distant areas normally encounter illnesses not frequent of their home nations, like Oropouche virus, which has spiked in 2024–25 amongst worldwide vacationers.
- Urbanization and Inhabitants Density: Since 2007, additional people dwell in cities than rural areas, creating crowded hotspots the place illnesses unfold like wildfire. The Nature Evaluations Microbiology highlights how metropolis growth amplifies transmission risks.
- Native climate Change: Rising temperatures and altering ecosystems are pushing vectors like mosquitoes into new territories, spreading illnesses like Zika and dengue. Evaluation in PLoS Neglected Tropical Sicknesses reveals temperature impacts on vector-borne sickness transmission.
- Zoonotic Spillover: About 60% of EIDs are zoonotic, meaning they leap from animals to folks. Deforestation and human encroachment into wildlife habitats improve these risks, as seen with Nipah virus and avian influenza, per the Nature Communications.
- Antibiotic Resistance: Overuse of antibiotics has birthed superbugs like multidrug-resistant tuberculosis, which the CDC flags as a rising menace.
Remaining 12 months, I traveled to a conference in Southeast Asia and seen firsthand how crowded markets and concrete sprawl blur the strains between folks and animals. A vendor casually talked about how bats, a acknowledged reservoir for viruses like Nipah, had been frequent in shut by forests. It hit me: our world is a petri dish, and we’re all part of the experiment.
The Worldwide Response: A Coordinated Effort
When a model new sickness emerges, the world doesn’t sit idly by. In 2025, worldwide responses to EIDs are additional delicate than ever, mixing science, protection, and experience. Nonetheless it’s not with out challenges. Proper right here’s how the worldwide neighborhood is tackling EIDs:
Surveillance and Early Warning Strategies
Catching a sickness early can indicate the excellence between a localized outbreak and a pandemic. Organizations identical to the WHO and the Worldwide Society for Infectious Sicknesses (ISID) run purposes like ProMED, a 24/7 early warning system that tracks sickness patterns worldwide. In April 2025, the Biothreats Emergence, Analysis and Communications Group (BEACON) launched its beta mannequin, using AI and worldwide skilled networks to watch outbreaks in precise time. This platform, housed at Boston School’s Coronary heart on Rising Infectious Sicknesses, is a game-changer for quick response.
I recall a dialog with a public properly being researcher who described ProMED as “the world’s properly being radar.” In 2024, it flagged early cases of Rickettsia sibirica mongolitimonae, a tickborne sickness rising in Europe, prompting swift movement in Spain’s reference labs. Surveillance isn’t practically info—it’s about saving lives.
Evaluation and Enchancment (R&D)
Rising vaccines, diagnostics, and coverings is a cornerstone of the worldwide response. The WHO’s R&D Blueprint prioritizes high-risk pathogens like MERS-CoV, Nipah, and “Sickness X”—an unknown pathogen that will spark the next pandemic. In China, R&D for EIDs has surged since 1990, with the Ebola vaccine Ad5-EBOV gaining emergency use authorization, as detailed in a CDC journal article. Within the meantime, the U.S.’s Biomedical Superior Evaluation and Enchancment Authority (BARDA) focuses on platform utilized sciences for quick vaccine development, a way that proved essential all through COVID-19.
The race for countermeasures isn’t low-cost or easy. My good buddy, a virologist, as quickly as shared how her crew labored throughout the clock to verify mRNA vaccine candidates all through the pandemic. “It’s like setting up a airplane whereas flying it,” she acknowledged. In 2025, enhancements like llama-derived nanobodies for SARS viruses, reported by ScienceDaily, current promise for future outbreaks.
Worldwide Collaboration
No nation can fight EIDs alone. The WHO’s Worldwide Properly being Legal guidelines (IHR) mandate information-sharing all through public properly being emergencies. In 2025, partnerships identical to the UK Properly being Security Firm’s (UKHSA) collaboration with worldwide researchers are enhancing genomic sequencing to hint pathogens like avian influenza. The UKHSA weblog highlights 24 priority pathogen households, urging additional R&D for coronaviruses and Nipah virus.
I as quickly as attended a worldwide properly being webinar the place a WHO official emphasised, “Collaboration isn’t optionally obtainable—it’s survival.” This rings true as nations share info on Oropouche virus, serving to map its 1–10-day incubation interval and inform journey advisories.
Public Properly being Interventions
From quarantine to vaccination campaigns, public properly being measures are essential. In 2024, Colorado reported a cluster of H5N1 avian flu cases linked to poultry publicity, prompting speedy contact tracing and isolation, per the Annals of Inside Medication. Neighborhood engagement, like Boston School’s partnership with the Museum of Science to teach most people, moreover performs a job in setting up perception and compliance.
Comparability Desk: Key EIDs in 2025
| Sickness | Pathogen Type | Main Space | Transmission | Key Response | Fatality Worth |
|---|---|---|---|---|---|
| Norovirus GII.17 | Virus | U.S. | Fecal-oral | Surveillance, hygiene campaigns | Low (<1%) |
| Oropouche Virus | Virus | Americas | Mosquito-borne | Journey advisories, vector administration | Low (<1%) |
| Rickettsia sibirica mongolitimonae | Micro organism | Europe, Africa, Asia | Tickborne | Doxycycline treatment, tick surveillance | Affordable (varies) |
| Streptococcus suis | Micro organism | South America | Zoonotic (pigs) | Meat safety guidelines, antibiotics | 4% |
| H5N1 Avian Influenza | Virus | Worldwide | Zoonotic (birds) | Poultry culling, vaccination | Extreme (as a lot as 50% in folks) |
This desk illustrates the number of EIDs and the tailored responses wished to deal with them, from hygiene campaigns to superior vaccine development.
Challenges inside the Worldwide Response
No matter progress, the fight in direction of EIDs faces hurdles:
- Helpful useful resource Allocation: Rising nations, normally EID hotspots, lack the surveillance infrastructure of richer nations. The Nature Communications analysis notes that worldwide properly being belongings are skewed in direction of developed economies.
- Antibiotic Resistance: Superbugs like Burkholderia thailandensis, which led to a lethal case in China in 2024, downside treatment protocols.
- Misinformation: Social media can amplify concern, as seen with unverified X posts a few supposed “$DEGE” SARS strain in July 2025. Such rumors complicate response efforts.
- Native climate and Biodiversity Loss: Environmental modifications drive zoonotic spillovers, however worldwide insurance coverage insurance policies normally lag behind.
I as quickly as seen a viral submit claiming a model new virus was “10x deadlier than COVID.” It took days for consultants to debunk it, nonetheless the panic had already unfold. Misinformation is a virus of its private, and in 2025, it’s a rising downside.
Actionable Advice for Folks
Whereas governments and organizations lead the fee, folks play a job too. Proper right here’s how one can defend your self and your neighborhood:
- Hold Educated: Observe trusted sources identical to the CDC and WHO for updates on outbreaks. Apps like ProMED’s mobile alerts can protect you inside the loop.
- Journey Good: Take a look at journey advisories on CDC’s journey properly being internet web page sooner than journeys, significantly to high-risk areas.
- Observe Hygiene: Widespread handwashing and meals safety practices can forestall illnesses like norovirus. I spotted this the laborious method after a stomach bug ruined a family journey!
- Get Vaccinated: Assure routine vaccinations, identical to the flu shot, are up-to-date. They’re your first line of safety.
- Help Conservation: Decreasing deforestation and supporting biodiversity can limit zoonotic spillovers. Donate to organizations identical to the World Wildlife Fund.
FAQ: Frequent Questions About EIDs in 2025
Q: What makes a sickness “rising”?
A: An rising sickness is each new to folks, rising in incidence, or spreading to new areas. Examples embrace SARS-CoV-2 and Oropouche virus, which have surged due to worldwide journey and environmental modifications.
Q: How does native climate change affect EIDs?
A: Hotter temperatures improve the differ of disease-carrying vectors like mosquitoes, whereas extreme local weather disrupts healthcare methods, making outbreaks harder to control.
Q: Can we predict the next pandemic?
A: Not precisely, nonetheless devices like WHO’s R&D Blueprint and BEACON’s AI surveillance help set up high-risk pathogens like “Sickness X.” Hotspots in tropical, biodiverse areas are fastidiously monitored.
Q: What’s the place of individuals in stopping EIDs?
A: Straightforward actions like vaccination, hygiene, and staying educated can reduce unfold. Supporting insurance coverage insurance policies for environmental security moreover helps forestall zoonotic illnesses.
Q: Are we larger prepared for pandemics in 2025?
A: Certain, due to advances in surveillance, R&D, and worldwide collaboration. Nonetheless, gaps in helpful useful resource allocation and misinformation keep challenges.
Conclusion: A Identify to Hold Vigilant
As I write this, I’m reminded of a late-night dialog with my grandfather, a retired doctor who lived by the polio interval. He acknowledged, “Medication is a race in direction of nature, and nature’s on a regular basis acquired a head start.” In 2025, that race is additional intense than ever. Rising infectious illnesses like norovirus GII.17, Oropouche virus, and H5N1 remind us that our world is interconnected, fragile, and persistently evolving. The worldwide response—by surveillance, R&D, and collaboration—is stronger than ever, however it certainly’s not foolproof. From AI-powered platforms like BEACON to grassroots education efforts, we’re setting up a sturdy safety. However, challenges like helpful useful resource disparities and misinformation protect us on our toes.
For readers, the next steps are clear: maintain educated, observe prevention, and advocate for insurance coverage insurance policies that strengthen worldwide properly being security. Whether or not or not it’s checking journey advisories sooner than your subsequent journey or supporting conservation efforts, every movement counts. The story of EIDs in 2025 isn’t practically pathogens—it’s about humanity’s resilience, ingenuity, and willpower to protect our shared future. Let’s protect working the race, collectively.
